Stanford School of Medicine, Stanford University Medical Center
Alexis B Hansen, B.A., Karen S Price, B.A., C.A.R. and Heidi M Feldman, M.D., Ph.D. Pediatrics, Stanford University School of Medicine, Stanford, CA, United States.
BACKGROUND
Cerebral Palsy (CP)
Definition
• Most common physical disability in childhood
• Affects 2-4 children/1000 ages 3 to 10 years
• Follows injuries to the fetal or infant brain
• Permanent, non-progressive neurological condition
• Peripheral effects of damage (i.e. spasticity) change as child grows
• Severity of CP classified using the Gross Motor Function Classification System (GMFCS): – Level I indicates minimal effects; Level V profound disability
Current treatments focus on reducing spasticity & improving function
• Oral medications
• Botulinum Toxin A (injection)
• Dorsal root rhizotomy (surgery)
• Tendon lengthening (surgery)
• Physical and occupational therapy
• Braces Recent research shows local changes in muscles and fascia in CP
• May contribute to pathogenesis and maintenance of spasticity
• Preliminary studies and clinical observations support the effectiveness of treatments directly targeting peripheral soft tissues
• There are few rigorous evaluations of such methods
Definition
• Specific manipulation technique developed by Ida P. Rolf PhD that focuses on putting body into alignment with the gravitational field
Philosophy
• Trauma (physical and emotional) and clinical conditions (cerebral palsy) create disorganized patterns of structure and function
• Once an imbalance exists, gravity exerts an unequal force on muscles and joints
• Fascia tends to magnify these effects through continued tightening in a chain reaction
• MSI manipulates muscles and fascia through pressure and deep tissue massage-like techniques to bring the soft tissues as close as possible to anatomically correct position
• Enhanced function occurs as a result of myofascial organization Protocol
• 10 sessions
• Therapist works on a different anatomical area each session to systematically treat the entire body
• Each session is approximately one hour
This study evaluates the therapeutic potential of Myofascial Structural Integration, a novel and safe technique of muscle and soft tissue manipulation, as a complementary treatment for children with spastic CP
Reproduced, with permission, from the Rolf Institute.
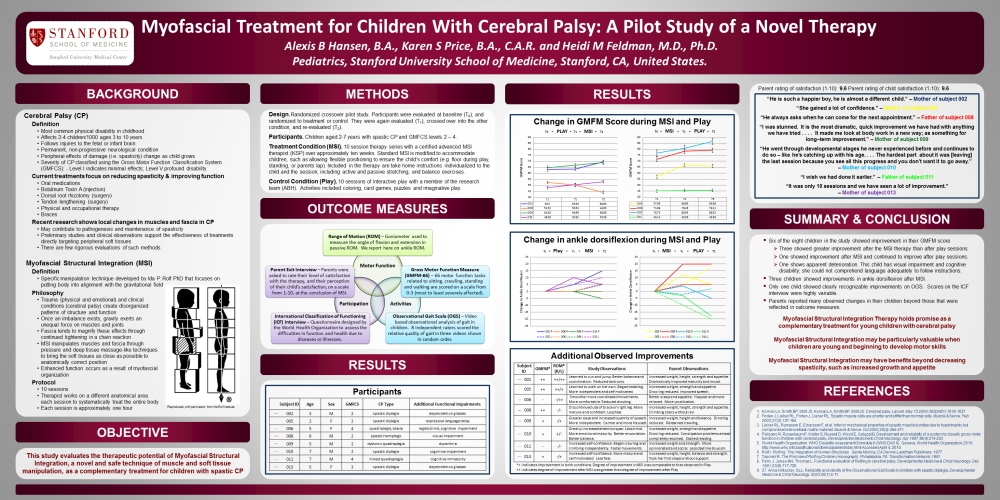
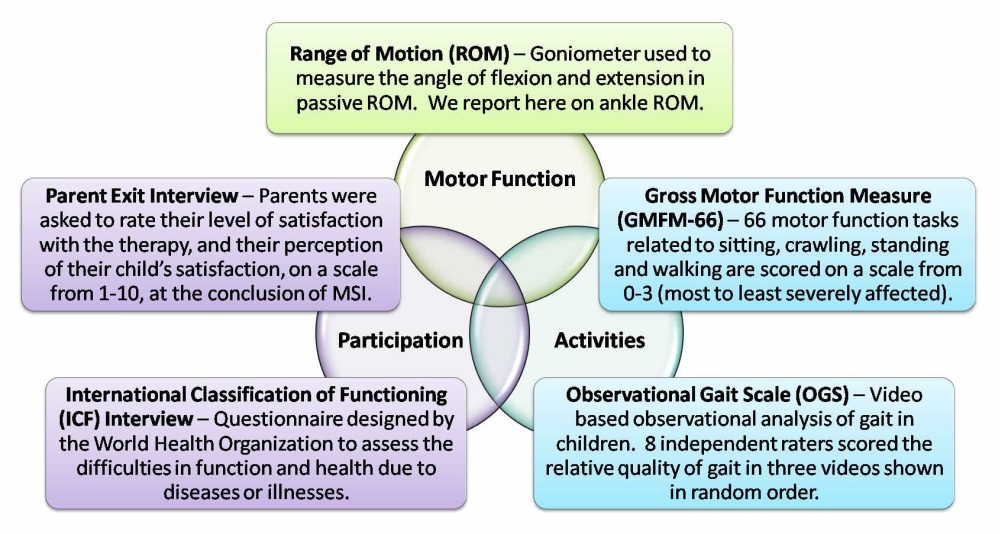
Design. Randomized crossover pilot study. Participants were evaluated at baseline (T0), and randomized to treatment or control. They were again evaluated (T1), crossed over into the other condition, and re-evaluated (T2).
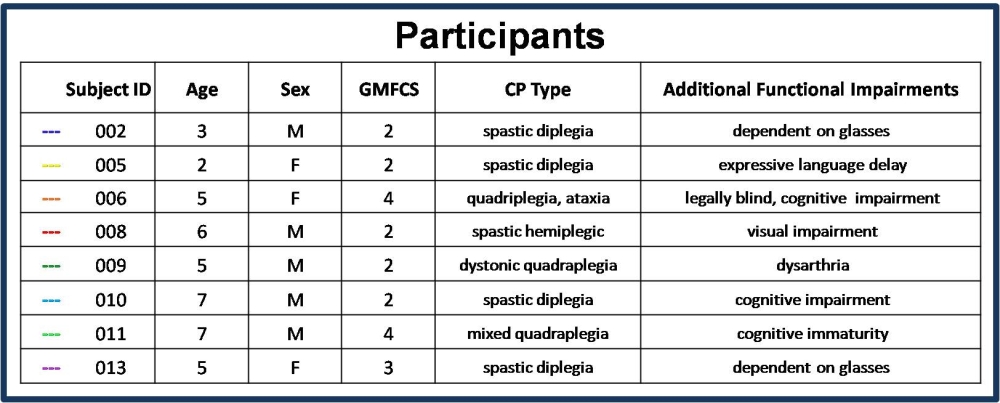
Participants. Children aged 2-7 years with spastic CP and GMFCS levels 2 – 4.
Treatment Condition (MSI). 10 session therapy series with a certified advanced MSI therapist (KSP) over approximately ten weeks. Standard MSI is modified to accommodate children, such as allowing flexible positioning to ensure the child’s comfort (e.g. floor during play, standing, or parents lap). Included in the therapy are take home instructions individualized to the child and the session, including active and passive stretching, and balance exercises.
Control Condition (Play). 10 sessions of interactive play with a member of the research team (ABH). Activities included coloring, card games, puzzles and imaginative play.
“He is such a happier boy, he is almost a different child.” — Mother of subject 002
“She gained a lot of confidence.” — Mother of subject 005
“He always asks when he can come for the next appointment.” — Father of subject 008
“I was stunned. It is the most dramatic, quick improvement we have had with anything we have tried… It made me look at body work in a new way; as something for long-term improvement.” — mother of subject 009
“He went through developmental stages he never experienced before and continues to do so — like he’s catching up with his age… The hardest part about it was [leaving] the last session because you see all this progress and you don’t want it to go away.” — Mother of subject 010
“I wish we had done it earlier.” — Father of subject 011
“It was only 10 sessions and we have seen a lot of improvement.” — Mother of subject 013
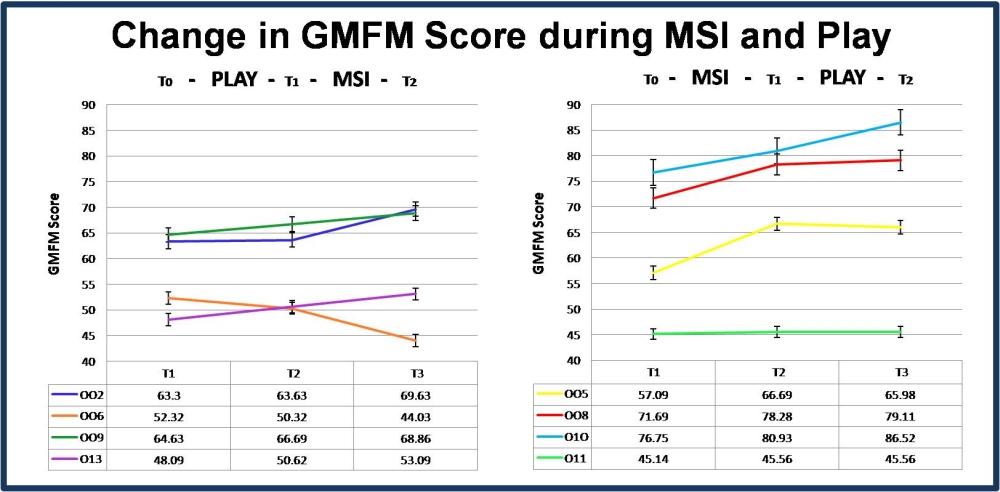
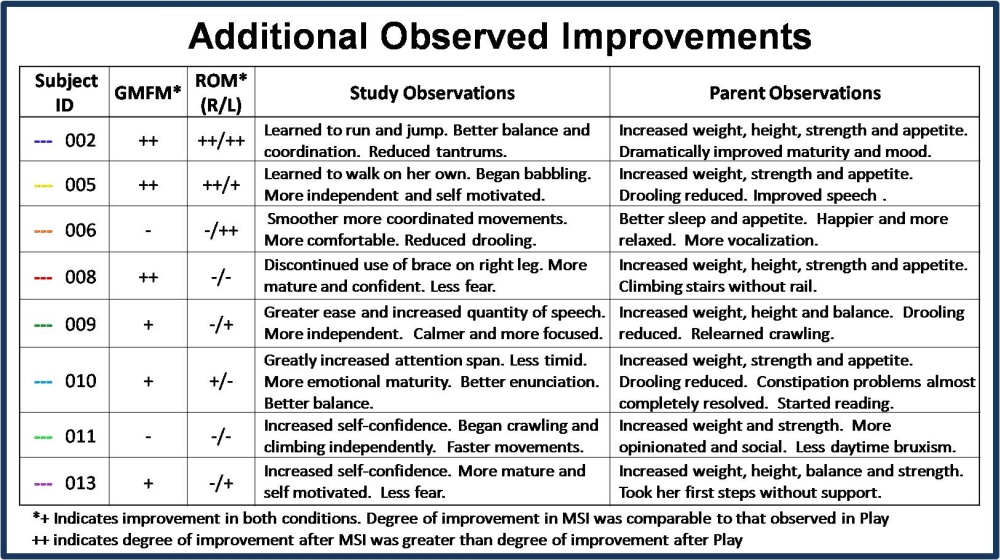
• Six of the eight children in the study showed improvement in their GMFM score.
• Three showed greater improvement after the MSI therapy than after play sessions.
• One showed improvement after MSI and continued to improve after play sessions.
• One shows apparent deterioration. This child has visual impairment and cognitive disability; she could not comprehend language adequately to follow instructions.
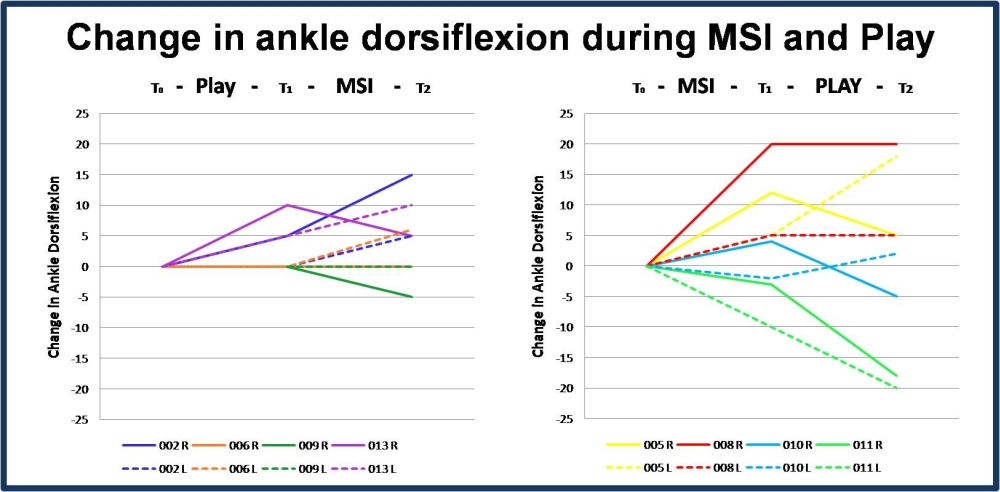
• Three children showed improvements in ankle dorsiflexion after MSI.
• Only one child showed clearly recognizable improvements on OGS. Scores on the ICF interview were highly variable.
• Parents reported many observed changes in their children beyond those that were reflected in outcome measures.
Myofascial Structural Integration Therapy holds promise as a complementary treatment for young children with cerebral palsy Myofascial Structural Integration may be particularly valuable when children are young and beginning to develop motor skills Myofascial Structural Integration may have benefits beyond decreasing spasticity, such as increased growth and appetite
1. Koman LA, Smith BP, Shilt JS, Koman LA, Smith BP, Shilt JS. Cerebral palsy. Lancet. May 15 2004;363(9421):1619-1631.
2. Friden J, Lieber RL, Friden J, Lieber RL. Spastic muscle cells are shorter and stiffer than normal cells. Muscle & Nerve. Feb 2003;27(2):157-164.
3. Lieber RL, Runesson E, Einarsson F, et al. Inferior mechanical properties of spastic muscle bundles due to hypertrophic but compromised extracellular matrix material. Muscle & Nerve. Oct 2003;28(4):464-471.
4. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine & Child Neurology. Apr 1997;39(4):214-223.
5. World Health Organization. WHO Disability Assessment Schedule II (WHO DAS II). Geneva: World Health Organization; 2010: http://www.who.int/classifications/icf/whodasii/en/index.html Accessed April 4, 2010.
6. Rolf I. Rolfing: The Integration of Human Structures. . Santa Monica, CA Dennis-Landman Publishers; 1977.
7. Toporek R. The Promise of Rolfing Children (monograph). Philadelphia, PA: Transformation Network; 1981.
8. Perry J, Jones MH, Thomas L. Functional evaluation of Rolfing in cerebral palsy. Developmental Medicine & Child Neurology. Dec 1981;23(6):717-729.
9. Anna H Mackey GLL. Reliability and validity of the Observational Gait Scale in children with spastic diplegia. Developmental Medicine & Child Neurology. 2003;45(1):4-11.
© Karen S. Price 2024 - - All Rights Reserved